Endoscopic Retrograde Cholangiopancreatography (ERCP)
in Denver, CO
What is an ERCP?
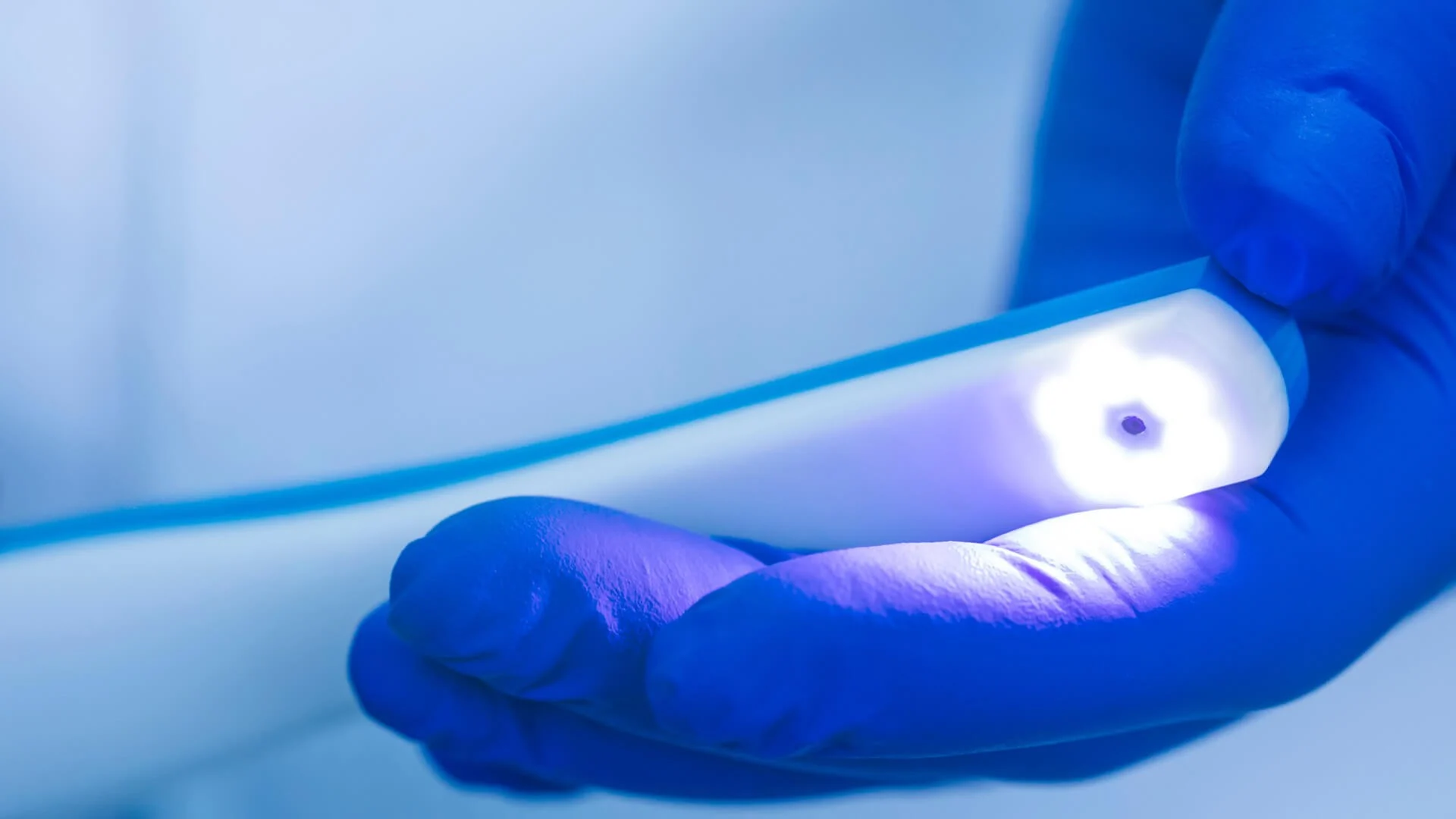
Denver Digestive Health Specialists perform endoscopic tests to assess several gastrointestinal (GI) disorders in patients. An ERCP, or endoscopic retrograde cholangiopancreatography, is an endoscopic process where a flexible, slender tube or “scope” is placed into the mouth and advanced to the first portion of the small intestine, known as the duodenum. The device is fitted with a camera and a light that enables the physician to evaluate the inner wall of the esophagus, stomach, small intestine, entrance to the bile duct, and pancreatic duct. Our GI team may conduct an endoscopic retrograde cholangiopancreatography assessment to diagnose the source of GI symptoms, such as:
- Abdominal pain
- Abnormal x-ray results
- Abnormal results from a liver test
- Pancreatitis
Call our Denver, CO practice today to request a visit with a gastroenterologist to hear more concerning an ERCP procedure.
What are the benefits of an ERCP?
An ERCP procedure may be recommended if blood tests reveal abnormal liver results, if you’re experiencing inflammation of the pancreas, or if you experience symptoms such as abdominal pain or yellowing of the skin and eyes. Some benefits of an ERCP test are:
- Diagnostic and therapeutic: This approach can serve two objectives, helping GI specialists diagnose conditions and provide treatment within the same procedure. As such, this can decrease the need to undergo multiple procedures.
- Enhanced precision: An ERCP helps enable the direct visualization of and treatment within the biliary and pancreatic ducts, which is crucial for accurate diagnosis and treatment.
- Short recovery periods: Patients often have faster recovery periods with an ERCP as opposed to traditional approaches involving surgery, allowing for a faster return to daily or routine activities.
- Efficiency: The ability to identify and treat a health issue within a single procedure often minimizes the overall treatment time.
How can I prepare for my ERCP procedure?
Before your ERCP, you will be given specific instructions from our team at Denver Digestive Health Specialists concerning what to expect and how to prepare. Most patients will be able to eat their normal diet the day before the test. Patients will be instructed not to eat or drink anything after midnight with the exception of any medications. It is very important to adhere to the instructions given by your provider. Further instructions surrounding your medications may be given. In general, your medication regimen will be followed as normal. In certain circumstances, particularly in patients on blood thinners, (for example Coumadin®, warfarin, Plavix®, aspirin, and anti-inflammatories) and with diabetic patients, special instructions will be administered.
What happens the day of the ERCP procedure?
Our staff will ask you to arrive at the endoscopy center in Denver, CO, 1 – 1.5 hours before your evaluation. This allows time to fill out patient forms and prepare for the evaluation. You will then need to change into a medical gown. An intravenous (IV) catheter will be placed in your arm so that sedation can start. Special equipment will also be used to permit the provider and our team to monitor your heart rate, blood pressure, pulse, electrocardiogram, breathing, and oxygen levels throughout and after the ERCP.
After entering the treatment room, you will lie on your stomach on the stretcher. Our GI specialists will then start the sedation solution. A small amount will be administered at a time to help ensure that you do not react to the sedative solution and to provide only the dosage you require. In comparison with other endoscopic evaluations, it is not uncommon for general anesthesia to be performed for an ERCP procedure. Once the necessary sedation level is established, the endoscope will be placed into the mouth. The endoscope will be gently moved through the esophagus and down into the stomach and small intestine where the pancreatic and bile duct empties into the small bowel. A small portion of air is administered via the scope into the digestive system to increase visibility. In an ERCP, an iodine-based contrast dye is introduced into the biliary duct and pancreatic duct. An x-ray imaging machine is utilized to take images of these structures to identify whether there are any irregularities. Any fluid remaining in the upper gastrointestinal tract can be removed by way of the scope. Depending on exam findings, a number of things could be conducted during the course of the assessment, including tissue extraction for a biopsy, opening the bile duct or pancreatic duct (sphincterotomy), removal of stones from the pancreatic ducts or gallstones from the bile ducts, or the placement of stents (plastic/metal tubes) into the bile or pancreatic ducts. Once the ERCP is complete, as much of the remaining fluid and air as possible will be suctioned out via the scope. The process takes between 30 – 90 minutes to complete based on the findings.
Once the test is over, you will be escorted to the recovery room to be monitored while the sedation medication begins to wear off. The dosage of sedation used during the ERCP and how you respond to the medication will affect how soon you wake up, but most patients are awake enough for release within 45 – 60 minutes. You will not be able to operate any vehicles for the rest of the day; therefore, you should arrange for a ride home in advance. You will also be directed not to sign important documents, work, or engage in strenuous activity for the rest of the day. In most situations, individuals can consume foods and beverages as usual after being dismissed from the endoscopy unit, but pertinent instructions concerning eating, activity, and medications will be administered prior to dismissal. On occasion, patients will be admitted to stay in the hospital overnight for evaluation or monitoring.
When will I get the results of my ERCP?
When the ERCP is complete, the provider and/or nurse will explain the assessment findings to you. The majority of individuals do not remember what is discussed after the process as a result of the effects of the sedation. Our Denver Digestive Health Specialists team strongly suggests you bring someone with you to whom the exam findings can also be explained, if possible. You will also be released with a typed report and will be contacted with any biopsy or other test results generally within seven days.
What are the risks of an ERCP?
In general, ERCP is known to be a very safe evaluation. In most situations, any complications that arise are not life-threatening. Should a complication occur, it may require hospitalization and surgery. Prior to beginning the procedure, the consent for treatment form will be discussed with the patient by the nursing staff. The provider will, again, discuss procedure risks before the exam initiates, and any concerns or questions can be discussed.
A condition referred to as acute pancreatitis, or inflammation of the pancreas is the most prevalent complication. This condition may affect 5 – 8% of cases, but the risk can be up to 20% depending on the individual. Pancreatitis signs and symptoms can include nausea, vomiting, abdominal pain, and possibly fever. Most cases are not severe and require four or fewer days in the hospital. While hospitalized, patients generally only need IV fluids and pain and nausea control. Rarely, however, pancreatitis can be more serious and even life-threatening.
Medication reactions associated with sedation can occur. These can include allergic reactions, difficulty breathing, heart and blood pressure effects, and irritation of the vein used to administer the medication. Bleeding may occur with biopsy procedures or a sphincterotomy. Again, significant bleeding, which could necessitate a hospital visit or blood transfusion, is not common.
The puncturing or perforation of the esophagus, stomach, or small bowel can take place. Such an occurrence may not be identified during the test, or remain unrecognized until a later time. In most cases, perforation of this type will lead to hospitalization and surgery. However, this is still a very uncommon complication, even when biopsies are taken or a sphincterotomy is performed.
In addition, in 5 – 10% of cases, the ERCP assessment might not be able to be carried out for varying reasons. It is very critical that the patient call the physician’s office promptly in the event any symptoms arise after the test, such as fever, worsening abdominal pain, or bleeding.
Similar to any other procedure, ERCP is not flawless. There exists a minor, acknowledged risk that health concerns, including cancers, can be missed during the procedure. It is critical to continually consult your healthcare providers as advised and bring any persistent or new symptoms to their attention.
Should you find yourself needing an ERCP in Denver, CO, our gastroenterologists can help you determine the optimal approach for your needs.
What are alternatives to an ERCP?
In certain cases, the alternatives are based on the intital reason for an ERCP. In the majority of cases, ERCP is the top option to evaluate and address certain problems in the biliary and pancreatic systems. However, an imaging technique referred to as a magnetic resonance cholangiopancreatography (MRCP), percutaneous transhepatic cholangiogram (PTC), or endoscopic ultrasound (EUS) or echo-endoscopy can also evaluate the bile ducts and pancreatic ducts. It is important to note that the MRCP is only a diagnostic procedure. Addressing any concerns will need to be accomplished through an endoscopic retrograde cholangiopancreatography or surgery. In addition, EUS or PTC do have treatment options.
ERCP FAQs
What questions might be helpful to ask your GI specialist about the ERCP procedure?
If you need an ERCP, you will probably have several questions or concerns or may not know where to start. Some common questions to ask your GI specialist may include:
- What might your GI provider anticipate finding during this process?
- What is the general success rate of an ERCP?
- In the event a complication occurs, are there any symptoms or signs you might experience?
What should you avoid doing after an ERCP?
You should avoid operating a vehicle for 24 hours after undergoing your ERCP, as the anesthesia can take that long to leave your body; therefore, it is essential to have a relative or friend plan to drive you home following your appointment. You may be instructed to hold off on eating for a some time, depending on the type of treatment that was conducted during your ERCP. Our team may also suggest that you take the rest of the day and potentially the following day off work. Our Denver Digestive Health Specialists team can help you understand what to expect before, during, and after the ERCP process.
What procedures can be performed during an ERCP?
An ERCP allows your GI provider to perform several different procedures. A few of the common treatments conducted during the ERCP process include:
- Placement of stents
- Biopsies (tissue sampling)
- Stone removal (bilestones)
- Sphincterotomy of the biliary sphincter
How can I prepare for an ERCP?
Our Denver, CO digestive health team can provide instructions for preparing for your ERCP procedure. However, a few directions you might need to follow are:
- Do not eat or drink for eight hours prior to your procedure. (Water may be okay to drink. Check with your doctor to confirm.)
- Avoid smoking for eight hours prior to your ERCP appointment.
- Give your GI provider a list of any prescription and nonprescription medications you are currently taking as well as any known allergies you may have.
